Having trolled the literature in an effort to consume and digest what has already been published in the name of "Pediatric Echo Normal Values" and "Pediatric Echo Reference Values" I have come to the conclusion that what I really wanted was this: a common collection of normative data, from which we could all draw our own conclusions.
That doesn't exist.
Yet.
There now appears to be growing and international interest in the matter of a common source of reference data for pediatric echo. An editorial (ePub ahead of print) in the European Journal of Echocardiography now is calling for:
immediate discussions of a universal standard...
a concerted and collaborative international approach...
a single study to allow z-score computation...
a robust set of normal values, derived from a large number of individuals...
I hope the European Society of Echo plans on discussing this similar matter with the American Society of Echo (or vice-versa) before things get too far along...
While it is looking like this project is in much more capable hands than my own (thankfully!), had I to do it myself it was going to be guided by one thing: data transparency.
Show me the data
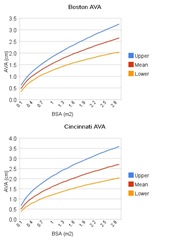
After having read some of the literature, I would occasionally find myself wondering "What if they had used a different BSA equation?", or "what if they had used height instead?" or used a different regression model, etc. For myself, I would love to see some of the studies re-done, but just slightly different.
Of course, nobody is going to do that— re-calculate their regressions— just because I, or you, want to see it done with our own particular and fanciful bias. And that is the point of a full disclosure database: DIY if you don't like this flavor. And, increasingly, I think that people will want to do just that. As an example, there is a preponderance of evidence that BSA, height, and weight are all inadequate for the purpose of scaling:
The cardiovascular system has evolved for effective distribution of metabolic substrates to tissue with high metabolic potential (Circ. 2008)
Cardiovascular structures scale with cardiac output and lean body mass.
In a very practical sense, there is no way to measure lean body mass (LBM) in the echo lab so the need for a good surrogate remains. Foster et. al., have already hinted at the concept of re-combining height and weight to better estimate lean body mass:
The combination of height and weight may provide a better surrogate for lean body mass than height alone, which could result in a superior prediction... This approach differs from normalization for body surface area; although body surface area equations include both height and weight, the particular combination of height and weight is lost once the surface area calculation is done.
Without providing open access to collected variables, like height and weight, any future data collection/analysis risks becoming irrelevant as our understanding of scaling cardiovascular structures evolves.
Show me more data
One of the biggest problems (IMHO) with the current approach to reference values is related to the matter of prediction. Different authors have proposed various methods of trying to predict the mean value of a given structure for a given body size, and these authors have similarly varied approaches to predicting the standard deviations. Understanding the relationship of the structure to body size is profound- and obviously important- but it is a different matter to determine if your measurement is normal- or not. For the purposes of reference values, the precise relationship of cardiac structure to body size doesn't matter.
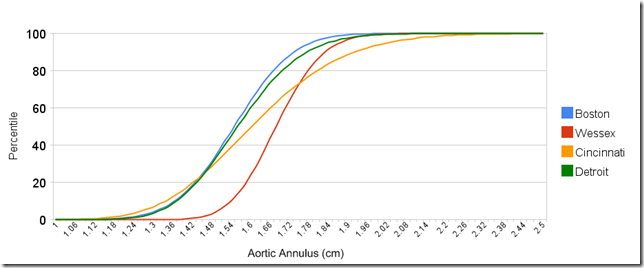
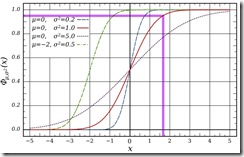
At its essence, a z-score has nothing to do with regression equations. Whenever we make an echocardiographic measurement, and consider its "normality" all we are really asking is "how does this measurement compare to the same measurement of normal subjects with similar size ?" That is, what is the mean and standard deviation of the same structure measured in a large group of similar-sized normal subjects?
The exact relationship and regression doesn't matter- as long as we have a collection of enough data on similar-sized subjects. What is required, though is... an awful lot of data, grouped in a meaningful way. The number of required subjects is daunting: grouped the way they did in their study (by height), an LV Mass reference database modeled after Foster et al., should probably have tens of thousands of subjects: 145 groups (47 to 191 cm, in 1 cm increments) x 100-200 subjects in each group (although, I would think the increment could safely be increased to 2 cm, thereby cutting the number of groups in half). This is why there is so much in the way of prediction: you need fewer patients. In spite of the huge numbers required, the study by Foster et al., is, or probably should be, the model for the future of echocardiographic reference values.
Even More Data
In the same way that our understanding of scaling of cardiovascular structures is evolving (height vs. BSA vs. LBM) , so too is our ability to measure these cardiovascular structures. Similar databases of reference values for the various Doppler modalities and 3D echo measures should be taken into consideration.
The architecture of this database could have long lasting effects. Designing a large database of common reference measurements for data transparency will allow us to continually make the most intelligent use of the tremendous effort required to collect this data.
- Normalization of echocardiographically derived paediatric cardiac dimensions to body surface area: time for a standardized approach.
- Kaski JP, Daubeney PE.
Eur J Echocardiogr. 2008 Sep 30. [Epub ahead of print] - Does size matter? Clinical applications of scaling cardiac size and function for body size.
- Dewey FE, Rosenthal D, Murphy DJ Jr, Froelicher VF, Ashley EA.
Circulation. 2008 Apr 29;117(17):2279-87. Review. - A novel method of expressing left ventricular mass relative to body size in children.
- Foster BJ, Mackie AS, Mitsnefes M, Ali H, Mamber S, Colan SD.
Circulation. 2008 May 27;117(21):2769-75. Epub 2008 May 19. - Interpretation of echocardiographic measurements: a call for standardization.
- Vasan RS, Levy D, Larson MG, Benjamin EJ.
Am Heart J. 2000 Mar;139(3):412-22.