A recent editorial states “In terms of practicality, developing normative values of right-heart dimensions by indexing to BSA is an important first step and should be encouraged.” If by “encouraged” they mean “discouraged and abandoned” then I totally agree.
An editorial in the December JASE discusses recent additions to the body of knowledge concerning reference values for the right ventricle:
Editorial:
- Hoit BD.
It's Time to Index the Right Ventricle, but to What and How?
J Am Soc Echocardiogr. 2012;25(12):1277-9.
Recent articles:
- D’Oronzio U, Senn O, Biaggi P, Gruner C, Jenni R, Tanner F, et al.
Right heart assessment by echocardiography: gender and body size matters.
J Am Soc Echocardiogr. 2012;25(12):1251–1258 - Willis J, Augustine D, Shah R, Stevens C, Easaw J.
Right ventricular normal measurements: time to index?
J Am Soc Echocardiogr. 2012;25(12):1259–1267 - D’Andrea A, Riegler L, Morra S, Scarafile R, Salerno G, Cocchi R, et al.
Right ventricular morphology and function in top-level athletes: a three-dimensional echocardiographic study.
J Am Soc Echocardiogr. 2012;25(12):1268–1276
That reference values for the right ventricle need to be improved is undisputed. However, I think the editorial went awry and gave some of the authors an undeserved pass.
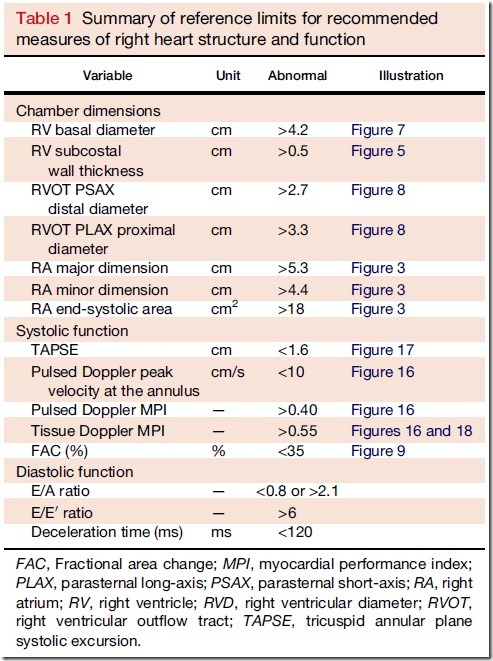
Firstly, as a matter of clarification, I believe the current guidelines for the right ventricle are unsuitable. Here’s why: they provide unscaled values:
In fact, the terms “scaled” and “body size” do not appear in the guideline document.
Anywhere.
Secondly, the editorial nicely details many of the shortcomings of indexing (i.e., heart size ÷ body size):
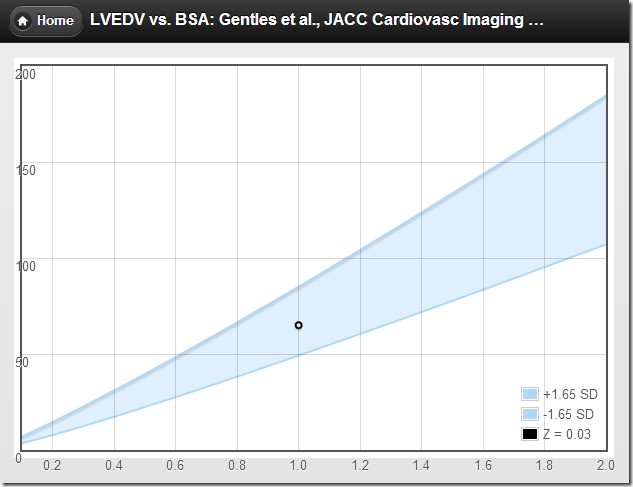
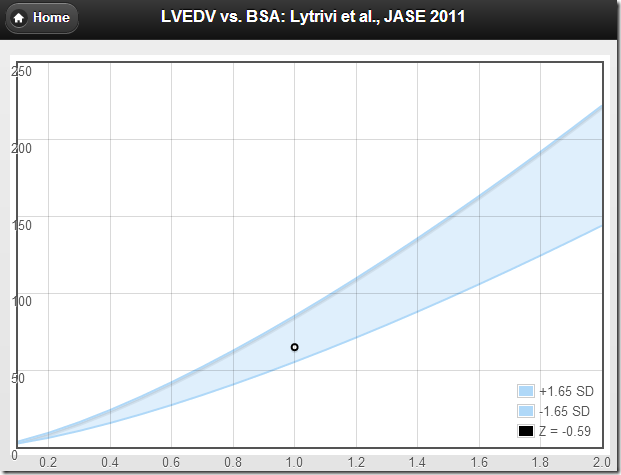
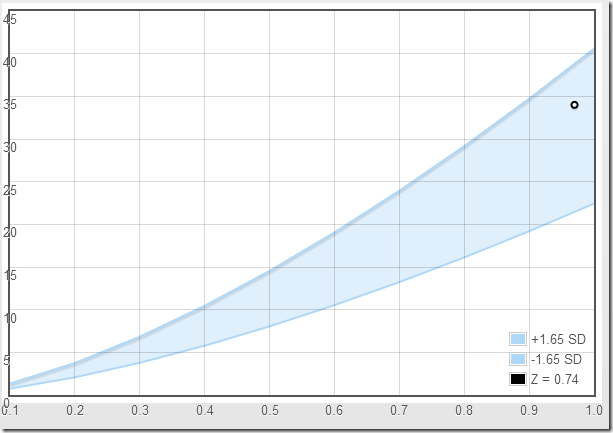
This approach is problematic for three reasons. First, the correlation between the cardiovascular parameter and body size may not be linear and may have unanticipated variation; second, difficulties may result when scaling a cardiovascular parameter to a body size parameter that has different dimensions (e.g., volume vs. area); and finally, it has been shown that ratiometric scaling does not produce size-independent scaled cardiovascular variables (i.e., the ratiometrically scaled variable (still) correlates with body size).
Yet the final assessment of the editorial is that indexed values are a “practical compromise”:
Indexing to BSA is a practical compromise but is inaccurate insofar as body composition affects the relation between body mass or surface area and cardiovascular variables; this problem may be particularly troublesome when normalizing dimensions in obese populations... In terms of practicality, developing normative values of right-heart dimensions by indexing to BSA is an important first step and should be encouraged.
There is some real truth in the problematic matter of using BSA as the size-adjusting parameter. The cardiovascular system has been optimized to deliver oxygen to tissues with a high metabolic need for it, i.e., lean body mass. Body surface area is a poor surrogate for LBM and, therefore, poorly represents the true relationship between body size, cardiac output, and organ size. But that is a problem for every attempt to scale heart size to body size, and not a unique problem for indexing. Indexing has it’s own flaws—fatal flaws—and couching those flaws in the terms of “BSA may be inadequate for obese populations” is misleading.
To be fair, the article by D’Andrea et al. understands the perils of indexing, and they should be recognized for their approach:
On the basis of the theoretical and empirical limitations of ratio scaling, we checked whether this scaling approach removed the influence of body size using a simple bivariate correlation approach. Where ratio scaling failed to remove the influence of body size, we subsequently investigated the nature of the allometric relationships between the BSA and 3D RV volumes and determined whether allometric scaling for the BSA provided size-independent RV dimensional indexes. Allometric scaling of the general form y = a * xb was used.
In my opinion, the most rational piece of work covering the matter is the fantastic editorial, Does size matter? Clinical applications of scaling cardiac size and function for body size. It is so relevant to the topic, it was cited in the current editorial 4 times. However, those authors arrived at the entire opposite conclusion:
indiscriminate use of ratiometric scaling approaches is at best problematic and at worst dangerous...
Reliance on parameters ratiometrically scaled to BSA for clinical decision making should be discouraged.
What we need in echocardiography is something of a reality check...
Stay tuned for that:
A Review and Critique of the Statistical Methods Used to Generate Reference Values in Pediatric Echocardiography.