lean body mass prediction equations based on height, weight, age, and gender are now available, providing insights into the practice of scaling of cardiovascular parameters to body size.
Recent critical reviews of reference values for pediatric cardiology are frankly sobering: we don’t have many studies with sufficient numbers of patients to draw reasonable conclusions, and the statistical methods are, at times, specious. I considered writing my own critical review of these critical reviews, but that just felt, well, a bit too
meta. Please read
this critical review of the many methodological limitations, and
this critical review of the statistical methods used in developing the current reference values. These are harsh but honest assessments of the current state of the art. Considering the criticism leveled against the community, it’s enough to make one wonder if anyone out there is even
trying to generate worthwhile reference data.
Clearly, some folks are.
Canadians, mostly, by the looks of things.
background
Since the very first time a pediatric cardiologist realized that babies weren’t just tiny adults, and that their hearts are small but proportional to their bodies, we have been in a struggle to figure out how best to adjust for body size. The usual suspects have all been tried, with varying success: age, height, weight, body surface area, various allometric exponents of the same... Some groups advocate that weight alone is the best scaling variable; others argue convincingly that height is better; other groups go back-and-forth between the two (see the works from Mass General:
2009 and
1992 ).
Combining both height and weight, BSA has proven to be quite good as a scaling variable, with a defensible theoretic and empiric case for it’s use (see
Sluysman and Colan, JAP 2005). But
why should cardiac size scale with height, or weight, or BSA? What is the underlying physical principle that says heart size should be proportional to height? Could it be because tall people breathe thinner atmosphere? Because heavy people have to deal with more friction?
Lean body mass (or “Fat Free Mass”-- our brain, bones, and primarily,
muscles) are what demand oxygen. If we were insects, we would just get our oxygen by moving the air right through our little exoskeletons. But most of us are not insects, and we get our oxygen instead via red blood cells, transported through our vast network of tubes, pumped from the heart.
The heart has developed to pump oxygenated blood to the tissues that need it.
“
Thank you very much, Captain Obvious” you say.
But there it is: the heart scales with lean body mass.
Yet, we don’t
measure lean body mass. Nobody in the echo lab measures LBM. In fact, it’s a rare person in the echo lab that even knows
how to measure it.
Traditionally, measurement of LBM required specialized equipment and training. Personally, I have never seen a pair of skinfold calipers in the cardiology department, and a dunk tank is almost entirely out of the question. I keep thinking a bioelectric impedance tool would somehow magically grow into this role, but I have yet to see that happen. Technically, I think you could measure it in the MRI scanner, but
DEXA is probably the gold standard, and I am pretty sure we don’t have one of those machines on campus.
Height and weight (and BSA) may be poor surrogates for LBM, but at least they are easy to measure.
recent work
In the
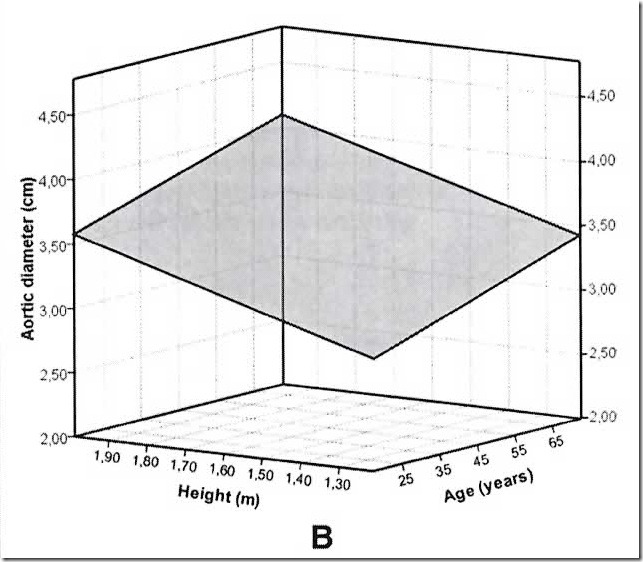
May-June issue of Annals of Human Biology, Foster et al. tackle the idea of developing a series of equations that could predict lean body mass from easily measured anthropometric measures. They measured lean body mass on over 800 children (using DEXA) and then performed some statistical kung-fu to develop their equations... and then validated those equations on another 300 or so patients. Using their prediction equations will get you within 5% of measured lean body mass, a feat that is about on par with some other available measurements (?bioelectric impedance??)
LBM estimated using this simple and inexpensive method may be useful in a variety of settings including ... characterization of the appropriateness of physiologic parameters that scale well to LBM such as resting energy expenditure, heart size, kidney function and drug dosing.
In an article in
the current issue of JASE, the same group now apply these new lean body mass prediction equations to the age-old question of how best to determine left ventricular hypertrophy, a matter which they had
previously covered and if I might add, raised the bar once already. They go on to demonstrate that— compared to values adjusted for lean body mass— height-adjusted LVM frequently over-estimates the incidence of LVH, and conversely, that BSA-adjusted values frequently under-estimate LVH (though less so than with height) They conclude the present investigation:
LBM is likely the best scaling variable and may be estimated reasonably accurately in children aged 5 to 21 years.
Only by scaling LV mass to LBM will we be able to determine the impact of obesity on heart size.
future directions
I think the ability to estimate LBM is going to be important to the field of reference values for echocardiography. It is, in effect, the
holy grail of scaling variables for pediatric cardiology, and cardiology in general.
I believe that this is going to be
so important to future research, I want to help you calculate lean body mass on your own data:
In an effort to be completely transparent about the calculations, I have also provided a step-by-step worked example lean body mass calculation:
And finally, a way to batch-process your data, adding lean body mass by the droves (upload your own csv data)